By Elizabeth Knight, PhD, DNP, FNP-C
By Elizabeth Knight, PhD, DNP, FNP-C
You’re dreading your next shift, and as you stare at the ceiling waiting for sleep, you think about calling out sick again. Work is not going well– everything and everyone is getting on your nerves. You get there late and don’t have time to get organized. You keep losing track of what you’re doing. You snapped at a patient the other day when he asked you a simple question. What’s going on? Where is the dedicated, competent, compassionate nurse you know you are?
You might be experiencing a condition known as compassion fatigue. Compassion fatigue is a state of emotional, physical, and spiritual distress triggered by the ongoing stress of caring for others who are sick or traumatized. It was first described in the scientific literature in reference to nurses (Joinson, 1992), and has now been identified in many types of caregivers. Though measuring compassion fatigue is difficult, research suggests that rates have been steadily increasing over the past ten years, and up to 50% of nurses experience it at some level. (Xie et al., 2021; Zhang et al., 2018). Let that sink in for a moment! Though you may feel isolated or even ashamed if you experience compassion fatigue, you are certainly not alone, and you’re not stuck with these feelings forever.
Why are nurses vulnerable to compassion fatigue? The word compassion comes from the Latin roots com- (together) and –pati (to suffer): it literally means “to share in suffering”. The nursing profession highly values compassion; for many nurses, it’s part of their self image and professional identity. For some, though, repeated exposure to suffering combined with therapeutic use of self can be draining. Compassion fatigue is most likely to develop when nurses believe their actions cannot make a difference, when they experience systemic problems like understaffing, and when they are not able to prioritize their own health and wellness. As the COVID-19 pandemic continues through its second year, the demands on nurses, both at work and at home, are intense and often overwhelming. Many have worked long hours and sacrificed their own safety, breeching personal boundaries out of a sense of duty. Combined with the stress of ongoing uncertainty, these conditions are a perfect storm for compassion fatigue.
Spotting Compassion Fatigue in Yourself and Others
Signs and symptoms of compassion fatigue can be psychological, behavioral, and physical. Psychological manifestations include reduced feelings of empathy, mood swings, irritability,  anxiety, anger, difficulty focusing, and a sense of dread. Associated behaviors include calling out sick and increased incidence of substance use. Physical symptoms include headaches, digestive problems, sleep disturbance, fatigue, chest pain, and palpitations (Lombardo & Eyre, 2011). Not everyone follows the same pattern, and there’s not a standard for diagnosis. You can also try a self-assessment found here: http://compassionfatigue.org/self-tests.html
anxiety, anger, difficulty focusing, and a sense of dread. Associated behaviors include calling out sick and increased incidence of substance use. Physical symptoms include headaches, digestive problems, sleep disturbance, fatigue, chest pain, and palpitations (Lombardo & Eyre, 2011). Not everyone follows the same pattern, and there’s not a standard for diagnosis. You can also try a self-assessment found here: http://compassionfatigue.org/self-tests.html
It’s easy to chalk symptoms like this up to garden-variety stress, or to blame yourself, or to think this is just a normal part of the job. It’s not. If you see yourself in the symptoms listed above, take it seriously.
Compassion Fatigue is Damaging to Health and Healthcare
In addition to the toll it takes on individual nurses, compassion fatigue hurts the entire healthcare system. Nurses in the throes of compassion fatigue are likely struggling to provide high-quality care. Mistakes, lack of empathy, and disrupted team dynamics can all negatively impact patients. Compassion fatigue can also contribute to understaffing, both acutely through absenteeism and long-term through nurses leaving the profession. This can in turn increase stress on nurses and perpetuate a vicious cycle.
Caregiving work like nursing is stressful and difficult, though this is often underrecognized. Nurses are not angels or preternaturally selfless people. They aren’t made of different stuff than everyone else. Nurses have needs, and employers should prioritize a culture promoting work-life balance, resources to support self care, and safe working conditions. Hospitals may rely on nurses’ sense of duty to patients to get them to work despite demanding hours, lack of time off, short staffing, and other modifiable factors. This needs to stop! Individual nurses experiencing compassion fatigue are not the problem– they are the evidence that something needs to change.

What to Do: Rescuing Yourself
Just like an injury to the body, compassion fatigue takes time to heal. It is not your fault and it is not something you need to hide. Start by recognizing that compassion fatigue is real, and it is not a permanent part of who you are. Though it can be tempting to seek immediate comfort, try not to rely on “counterfeit happiness” from things like alcohol, sex, social media, or drugs. Recognize that while you are suffering, you won’t feel better by blaming or complaining. Try not to make big decisions right away.
Here are some strategies you can try to start healing:
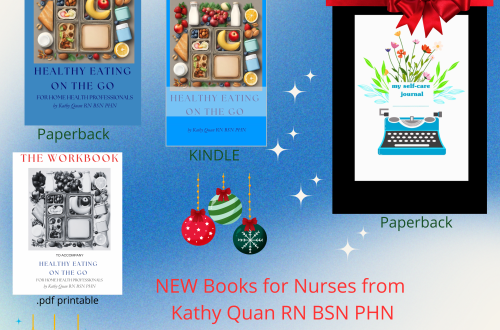
- Re-focus on lifestyle habits that feed resilience, including taking care of your physical body. Exercise, eat nourishing food, and spend time outdoors. Have you eaten fresh, delicious foods lately (and not just from the cafeteria or vending machine)? Are you well hydrated? Have you moved your body in a way that feels good? Consider working with a health coach to help you find a path forward in re-establishing healthy practices.
- Connect with loved ones. Make time for a phone call between shifts, a coffee date, or a “thinking of you” text. Nurturing relationships is healing for both people.
- Take time away from work. Don’t let unused vacation time expire. Don’t let yourself be bullied by real or imagined judgment from coworkers or management; the show can go on without you for a little while. As we might tell someone who’s lightheaded to sit down before they fall down, take time away before you are too ill to work.
- Consider a change of scene. Nursing is endlessly flexible. Is there an area of nursing you’ve always been interested in that you could explore? A different unit or setting can offer a fresh start, a different culture, and renewed energy.
- Work with a counselor or therapist to explore your emotional response to your work. Many workplaces have confidential employee assistance programs . Your health insurance may also cover counseling or psychotherapy.
- Recognize that there’s not an easy fix. Self-reflection and cultivating practices in line with your values can help, but it won’t fix things overnight. This kind of change takes dedicated, focused time working on yourself. Hospitals and other healthcare facilities don’t always make it easy to prioritize your own values at work, but taking time to center yourself, define your boundaries, and recommit to the reasons you were drawn to nursing in the first place are powerful practices you can do no matter what’s happening around you.
Remember that no matter what you decide to do for work, your compassion and empathy are strengths. Caring for others and caring for yourself are not mutually exclusive. Over time, it is possible to heal from compassion fatigue and develop meaningful, sustainable practices to support you in living in line with your values. You can’t take care of others if you don’t take care of yourself. To be authentic as a helpful healer, you must understand how to be healed.
References & Resources
Joinson, C. (1992). Coping with compassion fatigue. Nursing 22(4), 116, 118-119, 120. https://pubmed.ncbi.nlm.nih.gov/1570090/
Xie, W. et al. (2021). The prevalence of compassion satisfaction and compassion fatigue among nurses: A systematic review and meta-analysis. International Journal of Nursing Studies, 120. https://www.sciencedirect.com/science/article/pii/S0020748921001188
Zhang, Y. et al. (2018). Extent of compassion satisfaction, compassion fatigue and burnout in nursing: A meta-analysis. Journal of Nursing Management, 26(7), 810-819. https://onlinelibrary.wiley.com/doi/full/10.1111/jonm.12589
Lombard, B., & Eyre, C. (2011). Compassion Fatigue: A Nurse’s Primer. Online Journal of Issues in Nursing, 16 (1). http://www.compassionfatigue.org/
Further Reading
Ram Dass & Paul Gorman. How Can I Help? Stories and Reflections on Service.
The Caregiver’s Bill of Rights: https://compassionfatigue.org/uploads/1/3/7/9/137936581/cfap_caregiversbillofrights.pdf
Images free via Unsplash:
https://unsplash.com/photos/yIGinlYA6t8
https://unsplash.com/photos/YLmPK-XA1cM
https://unsplash.com/photos/jLWlA1HQMbE
By Elizabeth Knight, PhD, DNP, FNP-C
BIO: Elizabeth Knight is a family nurse practitioner, educator, and health coach in Portland, Oregon. You can find more of her writing at https://www.flowerpower.health/blog.
Thank Elizabeth for this great post!